Topic: Reducing ovarian cancer risk without removing the ovaries
A leading ovarian cancer organization has recommended that all women who have pelvic surgery should also consider removing their fallopian tubes to reduce their risk of ovarian cancer. (Posted 7/18/23)

RELEVANCE
Most relevant for: People who are not at high risk of ovarian cancer who are having pelvic surgery.
It may also be relevant for:
- healthy people with average cancer risk
- people with a genetic mutation linked to cancer risk
- people with a family history of cancer


Relevance: Medium-High
What is this about?
The Ovarian Cancer Research Alliance (OCRA) now recommends that all women who need pelvic surgery and have finished having children consider having their removed at the same time.
Why is this important?
No test or screening can detect for ovarian cancer at an early . For this reason, ovarian cancer is often not found until the later stages when it is harder to treat. One way to decrease your risk of ovarian cancer may be to have your removed while you are having pelvic surgery.
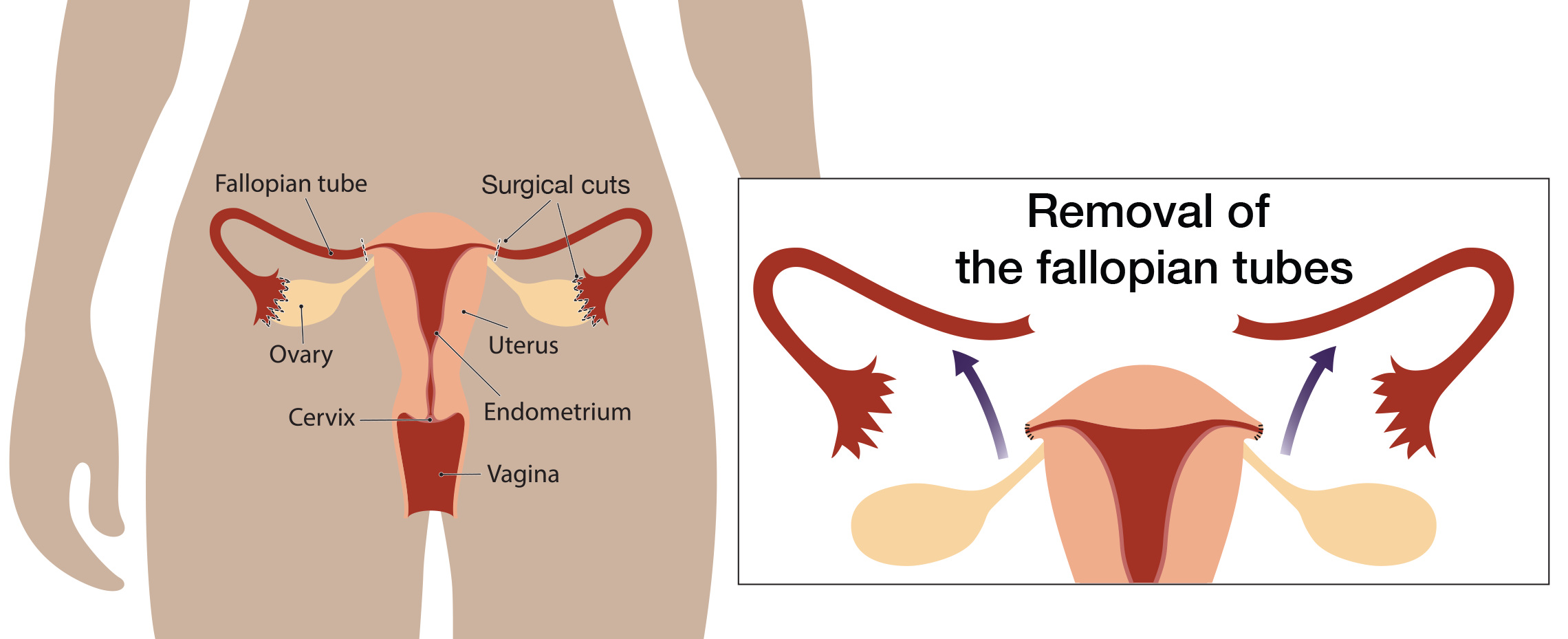
Most ovarian cancer starts in the , NOT in the ovaries
About 15-20 years ago, experts thought that most ovarian cancers started on the surface of the ovaries. However, more recent research has shown that most ovarian cancer begins in the . This discovery inspired researchers to study whether removing the (a surgery called ) after women are done having children lowers their risk for ovarian cancer.
Removing the during pelvic surgery
Many experts agree that for women of average ovarian cancer risk, removing the during another surgery in the pelvis (the area between the stomach and legs) is an effective preventive measure. Screening for ovarian cancer is not effective. Removing the to reduce ovarian cancer risk is already standard of care in Canada and other countries for women of average risk.
The new advice from OCRA recognizes that efforts to develop lifesaving screening tests for early detection of ovarian cancer have been unsuccessful and that women should consider more proactive measures.
Dr. Dianne Miller, a former leader of gynecologic cancer services in British Columbia, was quoted in the New Your Times:
“I remember the light-bulb-going-off moment that many of these cancers [ovarian] are likely preventable, because a lot of women have a surgery at some point for hysterectomy, or removal of fibroids, or tubal ligation.”
For women at average risk for ovarian cancer, Dr. Miller said that removing only the is a “win-win” situation, reducing ovarian cancer risk while the intact ovaries continue producing small amounts of hormones that help keep the brain and heart healthy later in life.
What about high-risk women?
Removing the ovaries and the is the most proven way to lower the risk of ovarian cancer in high-risk women. However, ovary removal has been linked to several risks, including increased heart disease, bone weakening, sexual side effects and other issues.
It is important to know that removing the while sparing the ovaries to lower ovarian cancer risk in high-risk women is still considered experimental. For high-risk patients who choose to have their removed first, removing their ovaries during the time period recommended by national guidelines is recommended. At the time of this review, research studies are ongoing to assess the safety of removing the first with delayed ovary removal. These studies are being done to see if this approach lowers the risk for ovarian cancer while minimizing the effects of menopause in high-risk women.
A study in the Netherlands found that people with a mutation have better quality of life after removal of only the with removal of ovaries later compared to removal of both ovaries and at the same time. You can read more about this study in our XRAY review here.
What does this mean for me?
High-risk women
If you are at high risk for ovarian cancer due to an , removing the ovaries along with the has been shown to significantly lower your risk for developing and dying from ovarian cancer. Current expert guidelines recommend removal of the ovaries and once you no longer plan to become pregnant, to lower your risk for cancer.
Ovary removal, even after menopause, has been linked to increased risk of heart disease, bone weakening, sexual side effects and other issues. If you are concerned about the side effects of surgical menopause or you are not ready to remove your ovaries, ask your surgeon if participating in a clinical trial studying removal of the with delayed removal of the ovaries might be right for you.
Average risk women
If you are a woman at average risk for ovarian cancer and are not planning on becoming pregnant in the future and need to have any type of pelvic surgery, you should ask your surgeon about the benefits and risks of removing your at the time of your surgery.
Reference
Rabin RC. “To Prevent Cancer, More Women Should Consider Removing , Experts Say.” The New York Times. Feb. 1, 2023.
Disclosure: FORCE receives funding from industry sponsors, including companies that manufacture cancer drugs, tests and devices. All XRAYS articles are written independently of any sponsor and are reviewed by members of our Scientific Advisory Board prior to publication to assure scientific integrity.
Share your thoughts on this XRAY review by taking our brief survey.
posted 7/18/23
The following are studies looking at ovarian cancer screening or prevention.
- NCT04251052: A Study to Compare Two Surgical Procedures in Women with Mutations to Assess Reduced Risk of Ovarian Cancer (SOROCk). This study is looking at whether women with mutations who remove just the can reduce the risk of ovarian cancer nearly as much as women who remove their ovaries and .
- NCT05287451: Risk Reducing With Delayed as an Alternative to Risk- Reducing Salpingo-oophorectomy in High Risk-Women to Assess the Safety of Prevention. This study will look at outcomes in women with , , , and who remove their , followed by removal of their ovaries compared to women who undergo standard-of-care removal of their ovaries and at the same time.
- Validating a Blood Test for Early Ovarian Cancer Detection in High-risk Women and Families: MicroRNA Detection Study (MiDE). The goal of MiDe is to develop a test to detect early-onset ovarian cancer. Currently, no reliable screening or early detection tests are available. Participants can be expected to provide up to 4 tubes of blood every 6 months for up to 5 years. These samples can be collected by mobile phlebotomy all around the US.
Additional clinical trials for ovarian cancer screening and prevention may be found here.
Updated: 04/10/2025
The following resources can help you locate an expert near you.
Finding gynecologists with expertise in cancer risk and treatment
- The Foundation for Women's Cancer has a search tool to help you find a gynecologic oncologist.
Related experts
Some symptoms and conditions related to female reproduction may be managed by other experts.
Fertility experts
- The Oncofertility Consortium maintains a national database of healthcare providers with expertise in fertility preservation and treatment of people who are diagnosed with cancer or have a high risk for cancer due to an .
- Livestrong has a listing of 450 sites that offer fertility preservation options for people diagnosed with cancer.
Financial assistance may be available to make the cost of fertility preservation affordable for more patients. Patients are referred to those programs as needed.
Menopause experts
- The North American Menopause Society has a tool to help you find a qualified menopause expert in your area.
Sexual health experts
- The Sexual Medicine Society of North America (SMSNA) has a search tool to find experts in your area who provide sexual health care services.
- The American Association of Sexuality Educators, Counselors and Therapists (AASECT) maintains a tool to help people find a sexual health expert near them.
Other ways to find experts
- The National Cancer Institute (NCI)-designated comprehensive cancer centers deliver cutting-edge cancer care to patients in communities across the United States. Most centers have specialized screening and prevention centers for high-risk people. Find a center near you and learn about its specific research capabilities, programs, and initiatives.
- Register for the FORCE Message Boards to get referrals from other members. Once you register, you can post on the Find a Specialist board to connect with other people who share your situation.
Updated: 04/09/2023