by Lisa Rezende, PhD (originally published in 2014 and republished in 2021 with a few updates)
Emerging research has linked having a BRCA1 inherited mutation with a small increase in risk for endometrial (uterine) cancer. In 2014, FORCE conducted a survey for women at high risk for ovarian cancer, to learn which factors influenced their decisions regarding whether or not to remove their uterus at the time of risk-reducing removal of the ovaries and fallopian tubes. Our survey was open to both women who had risk-reducing surgery and women who had not undergone risk-reducing surgery. The survey was accompanied by an overview of the research on the risk for endometrial cancer in women with BRCA1 mutations. Over 700 people responded. Here’s what you told us:
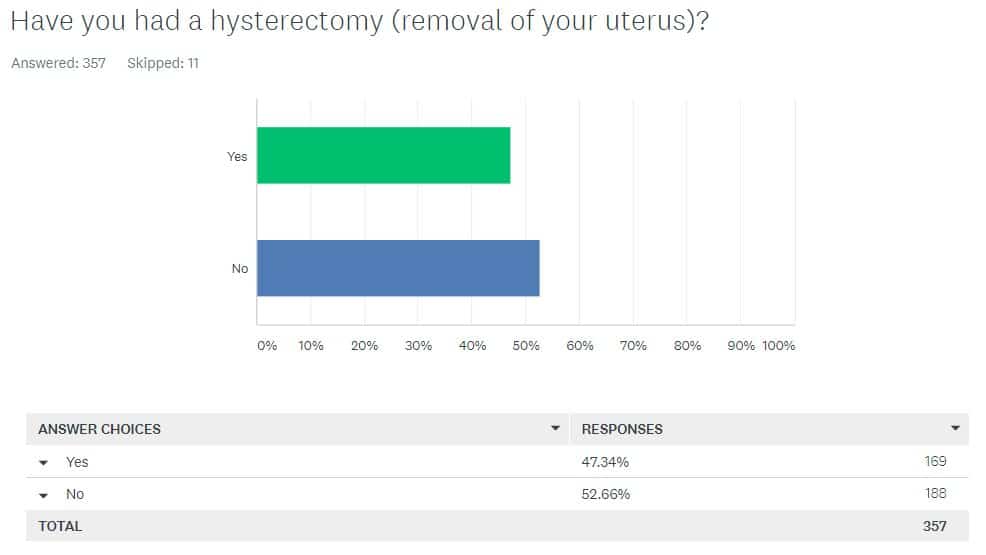
Our community is almost evenly split between those who kept their uterus and those who removed it.
One of the most striking findings is the near 50:50 split between women who removed their uterus (48%) and women who kept theirs (52%). The close split held up whether women had a BRCA1 or BRCA2 gene mutation. This lack of consensus is not surprising because currently no national guidelines exist on whether or not a BRCA mutation carrier should remove her uterus.1 In the absence of guidelines, women and their doctors make the choice together.
We asked what factors influenced your decision and we found that:
- for women who removed their uterus, the strongest factors influencing their decisions were:
- uterine cancer risk
- their doctor’s recommendation, and
- history of prior uterine abnormalities (such as fibroids)
- for women who did not remove their uterus, the strongest factors influencing their decisions were:
- their doctor’s recommendation
- the possibility of side effects from removing the uterus, and
- the possibility of surgical complications
If you had surgery, doctors’ recommendations weighed heavily in your decisions.
A doctor’s recommendation was the most cited factor that influenced whether a woman kept or removed her uterus: 49% of women who removed their uterus and 49% of women who kept their uterus said that their doctor’s recommendation strongly affected their decision. This speaks to the trust women have in their physicians, and the need to chose a health care team that specializes in high-risk women. This is an interesting finding, it makes sense that the opinions of physicians play a strong role in women’s health decisions. But in this case, doctors have no guidelines to follow2, and based on your reports, it appears that they are almost equally split in recommending for and against hysterectomy. We know very little about what is prompting these recommendations; a survey for health care providers could help answer this question.
We did not ask to what extent your personal preferences were taken into account by your physician. Future surveys and research will address the degree of shared decision making between patient and health care providers when making treatment decisions in the absence of clinical guidelines. From the survey, we did see that 13% of you kept your uterus despite doctor recommendations to remove it, and 3% of you removed your uterus despite doctor recommendation against hysterectomy.
Many of you mentioned in the comments that your insurance would only cover removal of ovaries and fallopian tubes for high-risk women. This speaks to the need to assure that insurance issues do not get in the way of informed shared decision making between physicians and patients.
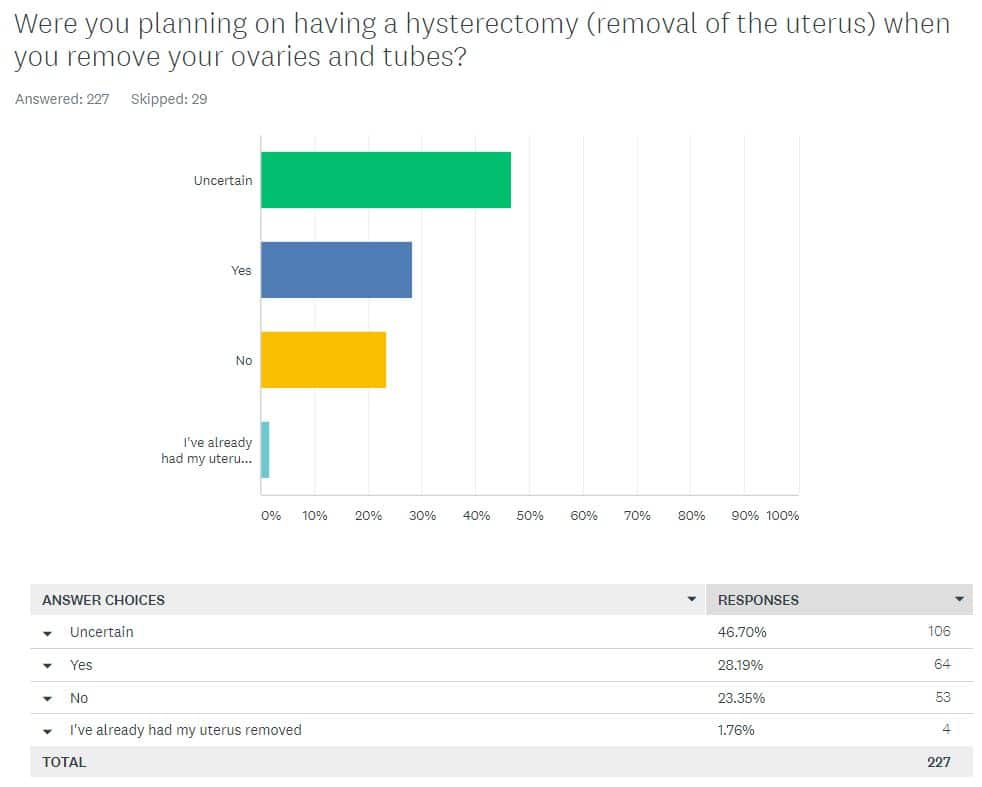
Many women are uncertain whether or not to remove their uterus when they have their ovaries and fallopian tubes removed.
We also asked women who are considering surgery whether or not they plan to remove their uterus as well. The largest group, 46% of women, remains undecided; 28% plan to remove their uterus; and 23% intend to keep their uterus.
The women identified the following factors that are likely to play a role in their decision:
- those who plan on removing their uterus cited as factors that are either strongly, or somewhat likely to influence their decision:
- risk of uterine cancer
- prior uterine abnormalities, and
- hormone replacement therapy
- those who plan to keep their uterus cited concerns that are either strongly, or somewhat likely to influence their decision:
- side effects
- possible surgical complications,
- longer surgery time
Women differ in how much uterine cancer risk is high enough to consider hysterectomy.
How high does your risk for uterine cancer have to be to consider hysterectomy? The answer is very individual. Women who responded to our survey varied widely in their tolerance for uterine cancer risk. The largest group of women, 19%, said they did not know at what risk they would consider hysterectomy. The article accompanying the survey found an estimated 4% lifetime risk of uterine cancer in BRCA1 mutation carriers. Interestingly, only 8% of women said a risk of 2-6% was sufficient to consider hysterectomy.
Pelvic exams are the most common follow-up care after surgery to remove ovaries.
Annual or twice-yearly pelvic exams are the most common follow-up care (in 75% of women) after prophylactic oophorectomy. Despite the lack of post-surgical screening guidelines, about 33% of women still have their CA-125 levels measured at least once per year, and 16% continue to have transvaginal ultrasound. Many women also expressed that they were unsure what follow-up care they should receive, and some noted that they had received different advice from different doctors.
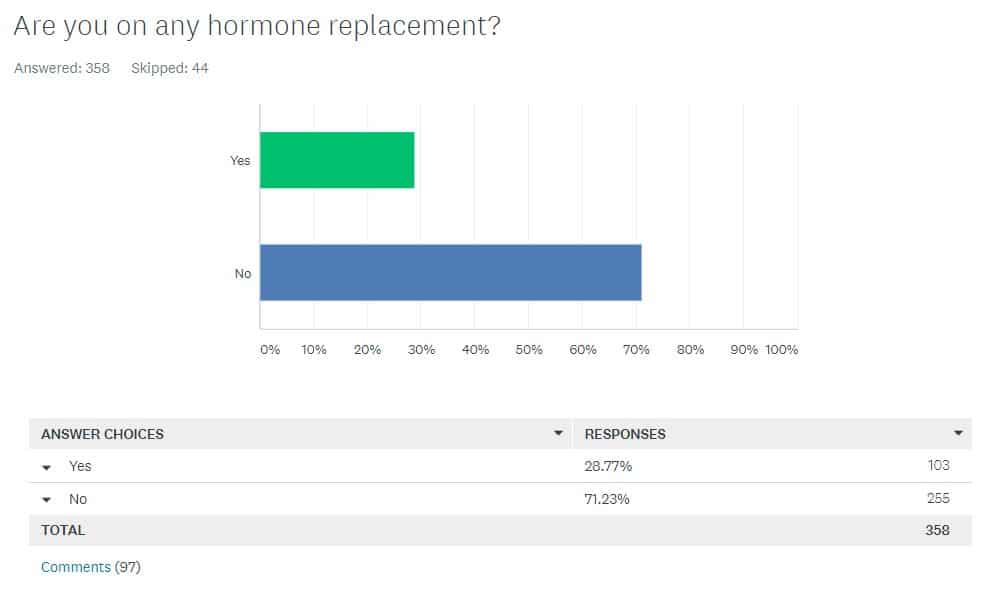
A majority of women do not take hormone replacement therapy.
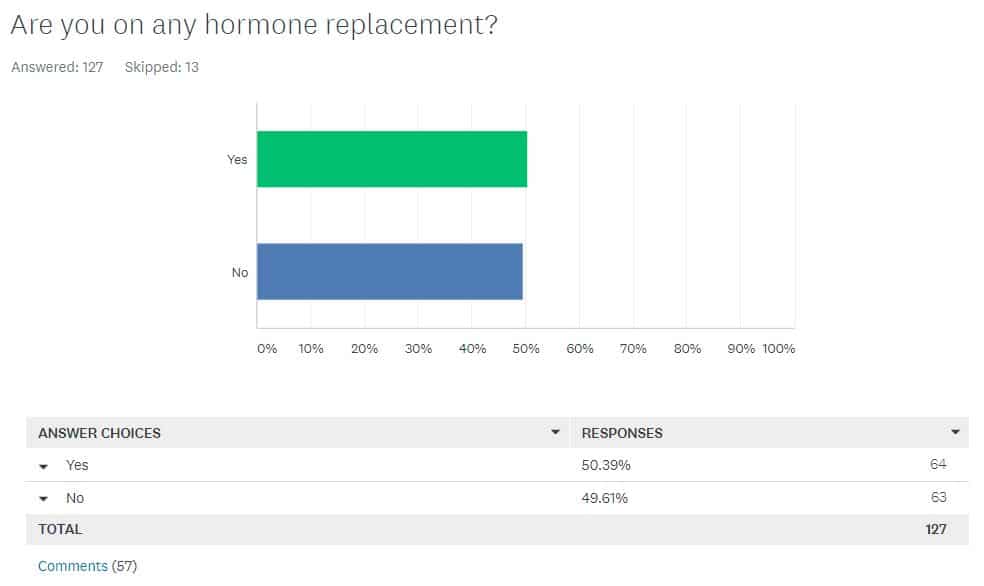
Another striking finding is the relatively low number only 28% of women who said they currently use hormone replacement therapy (HRT) after removal of their ovaries. This group included older women and breast cancer survivors who may not be good candidates for HRT. Among women under the age of 50 who had never had cancer, 50% were taking HRT and 50% of women were not. Future surveys will look deeper at the decision to take or forgo HRT.
Women indicated that after having BSO, reading a summary on uterine cancer risk changed their opinion on the health care decisions they made or might make in the future.
31% of women with BRCA1 mutations who had BSO without hysterectomy indicated that reading the article changed their opinion on health care decisions compared with 5% of women with BRCA2 mutations who had BSO without hysterectomy.
Women want more information on which to base their decisions.
When we asked which topics you felt needed to be addressed through research or more information to assist your decision-making, you said that you would like:
- more research and information on any link between BRCA2 and uterine cancer.
To date, no studies have definitively linked BRCA2 and uterine cancers. However, larger studies and longer follow-up time may be needed to find any small increase in risk. - more research information on quality of life and side effects of hysterectomy.
- more research and information on benefits and risks of HRT.
- information compiled and written in clear and easy to understand language.
- more research and better detection for ovarian cancer.
- more education for health care providers.
- more research on shared decision making between patients and health care providers
Several respondents felt that the risk for aggressive uterine cancer was so small that the report might cause unfounded fear and panic. The media, however, somewhat sensationalized the research. The Huffington Post’s headline, for example, stated, “BRCA Gene Mutation Could Also Raise the Risk of Deadly Uterine Cancer.”
Our article, which many said was clear and helpful in understanding the amount of risk for uterine cancer, is one of the topics that our members turn to FORCE for support or information.
We appreciate everyone who participated. Your responses will help us guide research and information where you tell us it is most needed. This survey has helped us determine that:
- more resources are needed to clearly explain the comparative benefits and risks for each medical decision associated with HBOC and provide balanced information on emerging research.
- more information is needed about how doctors make recommendations to patients in the absence of guidelines on a particular topic, particularly topics on which the medical community appears to be divided.
- more resources are needed to educate health care providers and insurance companies, and assure that women choosing hysterectomy have access to this service.
- more research is needed on long-term health and quality of life outcomes surrounding ovarian cancer risk and prevention in high-risk women.
- follow-up research is needed to understand how women make health decisions about hormone replacement.
1 Note, that although at the time of the survey there were not guidelines around hysterectomy with RRSO, current NCCN Guidelines as of 2021 include this statement: “The provider and patient should discuss the risks and benefits of concurrent hysterectomy at the time of RRSO for women with BRCA1 pathogenic/likely pathogenic variants prior to surgery.”