Stages and Subtypes
Read about cancer treatment options listed by gene mutation, type of cancer and type of treatment.Stay up to date on research and information
Sign Up for FORCE NewslettersBreast Cancer Stages and Subtypes
Cell types
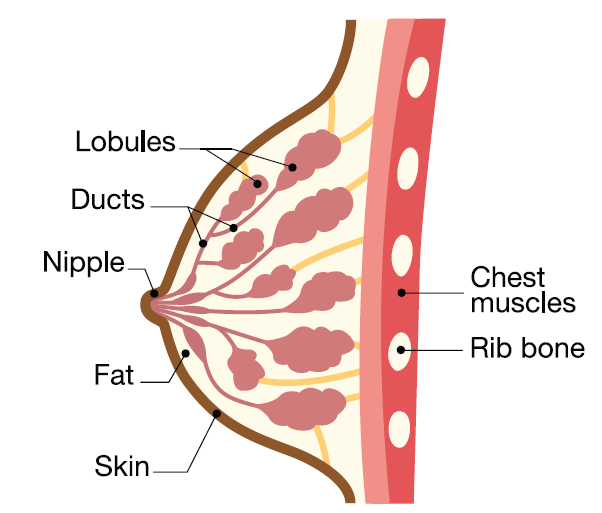
Breasts are made up of two main types of cells; the breast lobules, which make milk, and the breast ducts which carry the milk to the nipple.
- Ductal carcinoma is cancer that starts in the ducts. This is the most common type of breast cancer.
- Lobular carcinoma starts in the breast lobules. This is less common than ductal carcinoma.
In general, ductal carcinoma is more common than lobular carcinoma. However, people with inherited mutations in the gene are more likely to be diagnosed with lobular carcinoma.
Stages
The of a cancer refers to whether the cancer has spread beyond the breast, and if so, where in the body the cancer has spread. Measuring the of breast cancer helps doctors decide how to treat it. Breast cancer most often starts as a lump within the breast that can grow and spread:
- within the breast
- to nearby tissue (such as , skin or the chest wall)
- through the blood stream or lymph system to distant organs ()
During surgery, doctors will usually check one or more in the armpit to see if the cancer has spread. Doctors may also order tests such as chest XRAYS, , CT scans, bone scans or PET scans to learn if the cancer has spread beyond the breast and local lymp nodes.
In breast cancer, there are five major stages.
Stage |
Description |
Stage 0 (DCIS) |
A stage 0 breast cancer is known as a ductal carcinoma in situ (DCIS), a non-invasive form of the disease. The tumor cells are contained within the ducts of the breasts, and have not invaded beyond the duct. Cancers caught and treated at stage 0 are very unlikely to recur or spread. |
Stage 1 |
A small tumor (less than 2 cm) that is contained within the breast and has not spread to the lymph nodes. |
Stage 2 |
These cancers may be either: a) a larger tumor that involves the breast only, or b) a tumor that has spread to some lymph nodes in the armpit. |
Stage 3 |
These breast cancers may be either a) a tumor in the breast that invades the skin or chest muscle, or b) a tumor that involve several lymph nodes surrounding the breast (in the armpit, near the collarbone, near the breast bone). Some stage 3 breast cancers are considered “locally advanced.” |
Stage 4 (metastatic) |
These breast cancers have spread beyond the breast and the regional lymph nodes to another place in the body, such as the bone, lung, and/or liver. Stage IV breast cancers are also called “advanced” or “metastatic.” |
Stages of breast cancer |
|
Most breast cancers diagnosed at stages 0-3 are considered "," because they are curable. breast cancer is often treatable at diagnosis. Over time, breast cancer is likely to progress or recur; sometimes after several different types of treatment. There are many different treatments available for breast cancer, and clinical trials testing new treatments are often available.
Subtypes and biomarkers
After a biopsy or surgery confirms breast cancer, pathologists look closely at the cells for additional clues on how to best treat the cancer. All breast cancers are tested for common changes, called tumor biomarkers: receptor (ER), progesterone receptor (PR), and . The results of these tumor tests play a major role in choice of cancer treatment:
Hormone receptor ( or ER/PR) testing
- Doctors use hormone receptor tests to measure if cancers are "hormone sensitive" and might respond to hormone therapy. Doctors may refer to these tests as hormone receptor tests ( tests) or and progesterone receptor tests (ER/PR tests). In general, they refer to the same test.
- or ER/PR-positive: breast cancers with these biomarkers are called "hormone sensitive" breast cancers. These are usually treated with hormone therapy. Hormone therapy may be combined with chemotherapy or depending on the of the tumor and other factors.
- HR-negative or ER/PR-negative: these are almost always treated with chemotherapy and, or , because hormone therapy does not work well for these types of tumors.
testing
- Doctors use a test to measure the amount of a protein called on the surface of cancer cells. Cancers with a large amount of protein are called . These cancers often respond to certain types of targeted therapies.
- test results range from 0 to 3+.
- HER2-positive: A tumor with a score of 3+ is considered . These cancers are often treated with a type of known as "anti-HER2 therapy." Common anti-HER2 therapies include Herceptin (trastuzumab) and Perjeta (pertuzumab). Anti-HER2 therapy may be given with chemotherapy for people with , curable tumors. People whose tumors are and ER-positive receive hormone therapy, as well as chemotherapy and anti-HER2 therapy.
- HER2-low: In the past, a tumor with a score of 0 to 1+ was called and a score of 2+ was considered borderline. Updated scoring labels tumors with 1+ and 2+ as "HER2-low." Some people with advance or breast cancer that is HER2-low may benefit from an anti-HER2 therapy known as Enhertu (trastuzumab deruxtecan).
- HER2-negative: A tumor with a score of 0 is considered .
HER2 Score |
HER2 Status |
Score is 0 |
Tumor is HER2-negative |
Score is 1+ or 2+ |
Tumor is HER2-low |
Score is 3+ |
Tumor is HER2-positive |
Possible HER2 test results and meaning |
|
- Triple-negative breast cancers: tumors that are negative for all three markers (ER, PR and ) are referred to as or for short. Triple-negative breast cancers are almost always treated with chemotherapy.
Additional tests can be performed on tumor samples or blood to help guide treatment.
- For people with ( 1 or 2) cancer, prognostic tests can help guide decisions about chemotherapy and hormone therapy. These tests include Oncotype DX, MammaPrint, and Prosigna.
- For people with advanced cancers, tumor testing can look for additional biomarkers to help guide the choice of targeted therapies.
The following organizations offer peer support services for people with, or at high risk for breast cancer:
- FORCE peer support:
- Our Message Boards allow people to connect with others who share their situation. Once you register, you can post on the Diagnosed With Cancer board to connect with other people who have been diagnosed.
- Our Peer Navigation Program will match you with a volunteer who shares your mutation and situation.
- Connect online with our Private Facebook Group.
- Join our virtual and in-person support meetings.
- Other organizations that offer breast cancer support: